Syllabus: GS2/Health/GS3/Economy
Context
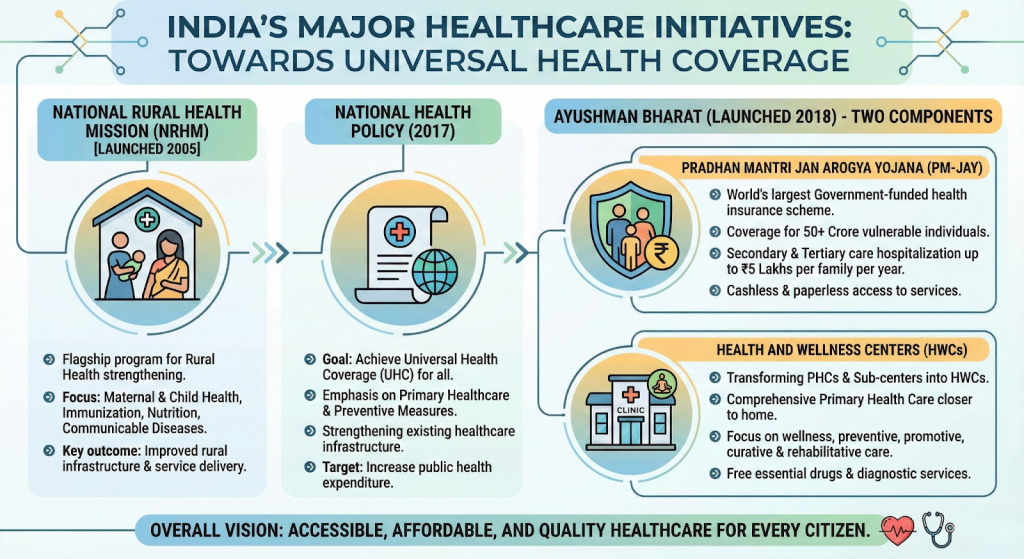
- India committed to Universal Health Coverage (UHC) through the National Health Policy (NHP), 2017 and SDG-3, operationalised mainly via Ayushman Bharat (AB).
- Despite progress, India continues to face a serious access–affordability–quality gap, indicating that UHC goals remain underachieved.
What is Universal Health Coverage?
- It means that all people have access to the full range of quality health services without financial hardship.
- Key components of UHC include:
- Access to Care: Everyone should be able to obtain necessary health services when they need them.
- Quality Services: The care provided should be effective, safe, and of good quality.
- Financial Protection: Individuals should not face financial difficulties due to medical expenses.
- UHC is rooted in the universal human right to health, affirmed in international covenants and the Alma-Ata Declaration (1978), which prioritised comprehensive primary healthcare.
Need For Universal Health Coverage in Indian Context
- Historical Commitment to Universal Healthcare:
- Bhore Committee (1943–46) reflected a clear preference for universal healthcare over insurance-based UHC.
- Policy Evolution after Independence:
- India’s National Health Policy of 1983 recognized the goal of “Health for All” and emphasized the importance of primary healthcare and equitable distribution of healthcare resources.
- Shift towards Insurance-led UHC:
- Welfare Schemes like Rashtriya Swasthya Bima Yojana (RSBY) 2008 and Ayushman Bharat–PMJAY institutionalised UHC but reinforced an insurance-heavy approach.
- Weak Public Health System and Rising Private Dependence:
- Chronic underfinancing of primary healthcare has led to poor quality public provisioning, shortage of infrastructure and workforce.
- National Sample Survey (NSS) data show growing reliance of the poor on private healthcare, rising out-of-pocket expenditure (OOPE) & increased household indebtedness.
- Constitutional Basis for UHC:
- The Directive Principles of State Policy in Part IV of the Constitution provides a basis for the right to health.
- Article 39 (e) directs the state to secure the health of workers; Article 42 emphasises just and humane conditions of work and maternity relief; and Article 47 casts a duty on the state to raise the nutrition levels and standard of living, and to improve public health.
- The Constitution also endows the panchayats and municipalities to strengthen public health under Article 243G.
- Post-Covid Realisation:
- The Covid-19 pandemic exposed inequities in insurance-based access, exclusion of informal workers and migrants & fragility of hospital-centric models.
- Present Policy Direction:
- Currently, India aims to attain UHC through the expansion of the Ayushman Bharat-Pradhan Mantri Jan Arogya Yojana (AB-PMJAY), the flagship publicly financed health insurance (PFHI) scheme of the Union government.
Challenges in Adopting UHC in India
- Resource Constraints: India faces significant funding limitations in healthcare, with a low public health expenditure compared to many other countries. This affects the ability to provide comprehensive services.
- Low public health expenditure (~2.1% of GDP), below the NHP target of 2.5%.
- Infrastructure Gaps: Many areas, especially rural regions, lack adequate healthcare infrastructure, including hospitals, clinics, and trained personnel, making access to care difficult.
- Healthcare Workforce Shortages: There is a shortage of healthcare professionals, particularly in rural areas, leading to disparities in access and quality of care.
- Fragmented Health Systems: India’s healthcare system is a mix of public and private providers, leading to inconsistencies in quality and accessibility.
- And, Health is a State subject, while financing and flagship schemes are centrally driven, leading to uneven outcomes.
| Lessons from Global Experience – WHO Alma-Ata Declaration (1978) emphasised primary healthcare as the foundation of UHC. – Several East Asian countries adopted UHC through an insurance approach, but have also strengthened primary and secondary care over time. a. An ageing population and chronic diseases have necessitated such changes. – Countries like China and South Korea achieved near-universal insurance coverage but faced high fiscal costs. – Recognising sustainability issues, China shifted strategy towards: a. Strengthening primary and secondary care. b. Emphasising prevention, early detection, and follow-up. c. Investing in human resources and population outreach. d. A strong public sector helped regulate private providers, though private influence remains a challenge. |
Making Ayushman Bharat 2.0 More Effective
- Shift from Coverage to Care: Move from hospitalisation-centric insurance to universal healthcare.
- Strengthen comprehensive primary healthcare as the first point of contact.
- Strengthen Primary and Secondary Care: Invest in infrastructure, diagnostics, medicines and referral systems.
- Use HWCs as gatekeepers to reduce avoidable hospitalisation.

- Increase Public Investment: Raise health spending to at least 2.5% of GDP.
- Prioritise preventive and promotive care and social determinants of health.
- Digital and Human Resource Reforms: Integrate ABHA ID, interoperable health records and disease surveillance.
- Address workforce shortages through task-shifting, local recruitment and continuous training.
- Better Regulation and Strategic Purchasing: Standard treatment guidelines, cost controls and accountability mechanisms.
- Align insurance schemes within a strong public health system, as seen globally.
| Daily Mains Practice Question [Q] Financial protection without strong public health provisioning can deepen healthcare inequities. Examine |
Source: IE
Previous article
Courts Must Protect, Not Regulate Free Speech