Syllabus: GS2/Polity/Health/GS4/Ethics
Context
- The U.K. House of Commons passed the Assisted Dying Bill to allow terminally ill people in England and Wales to end their lives.
About
- The bill will only apply to people in England and Wales who have less than six months to live.
- A patient choosing to die would need to be of competent mind and two doctors, a psychiatrist, senior lawyer and social worker would need to sign off on their decision.
- Advocates regard the new Bill as a humane and compassionate intervention that brings closure to a painful dependence on the immediate family.
- Opponents are apprehensive that the severely disabled and vulnerable patients may feel forced to end their lives to relieve the burden on relatives.
What is Assisted Dying?
- Assisted dying refers to the act of helping someone intentionally end their life, typically to relieve suffering from a terminal illness or severe, untreatable pain.
- There are two main forms:
- Assisted Suicide: A person, with the help of a medical professional or another person, takes their own life, usually by consuming a prescribed lethal dose of medication.
- Euthanasia: A doctor or healthcare provider actively administers a lethal substance to end the life of a patient, typically at their request, to relieve extreme suffering.
Status Across the Globe
- The practice of assisted dying is highly controversial and is legal in only a few countries or regions, with strict guidelines and regulations where it is permitted.
- Switzerland was the first country which in 1942 legalised assisted dying.
- Across Europe, six countries have some form of legalised assisted dying: Switzerland, the Netherlands, Belgium, Luxembourg, Spain and Austria.
- Later on the U.S., Australia and New Zealand enacted related legislations.
- Canada’s 2016 Medical Assistance in Dying law may be availed even by those whose condition is not terminal.
What is the position in India?
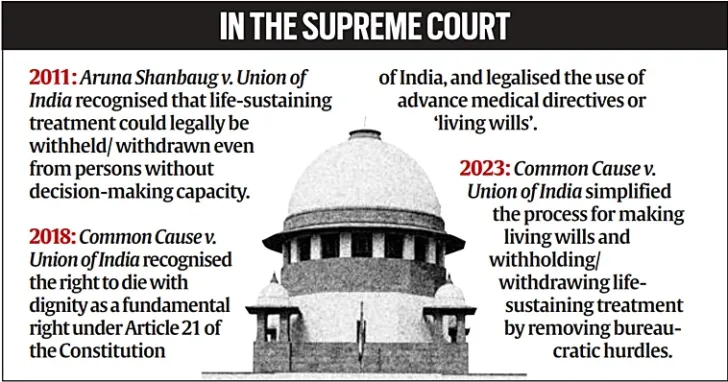
- The Supreme Court had in 2018 legalised passive euthanasia, contingent upon the person having a “living will”.
- SC held that the ‘right to die with dignity’ forms a part of the right to life under Article 21 of the Constitution of India.
- A living will is a written document that specifies the actions to be taken if the person is unable to make their own medical decisions in the future.
- Goa is the first state that has formalised, to some extent, the implementation of directives issued by the Supreme Court.
- In 2024, the Health Ministry released draft guidelines on withdrawing medical support for terminally ill patients.
- These specify that doctors must refrain from initiating life-support measures when they offer no benefit to the patient and are likely to cause suffering and a loss of dignity.
Arguments in Favour of Assisted Dying
- Autonomy and Choice: Individuals should have the right to make decisions about their own lives, including the choice to end it to avoid prolonged suffering.
- Relief from Suffering: Assisted dying provides a compassionate option for those with terminal illnesses or unbearable pain, allowing them to die with dignity.
- Quality of Life: For some, the quality of life may deteriorate to a point where death is seen as a better option than living with constant suffering or loss of independence.
- Respect for Individual Rights: People should have control over their bodies and lives, including the decision to end their life in a humane and controlled manner.
Arguments Against Assisted Dying
- Moral and Ethical Concerns: Many believe that taking a life, even at the person’s request, is morally wrong and goes against the sanctity of life.
- Risk of Abuse: Vulnerable individuals, such as those with mental health issues or pressure from family, may be coerced into choosing assisted dying.
- Medical Ethics: Healthcare professionals are traditionally bound to preserve life, and assisted dying may conflict with the fundamental role of doctors in healing and care.
- Alternative Solutions: Advocates argue that palliative care and pain management can provide relief, making assisted dying unnecessary.
Way Ahead
- Stronger Regulations: Implementing strict legal safeguards to ensure it is only available to those who meet specific criteria.
- Palliative Care Expansion: Improving access to high-quality palliative care to address suffering and reduce the demand for assisted dying.
- Public Debate: Ongoing discussions about the moral, legal, and ethical implications of assisted dying, can be considered while framing the guidelines.
- International Perspective: Countries may look to those with legal assisted dying frameworks for guidance on effective regulation and safeguards.
- Mental Health Support: Providing psychological evaluations to prevent coercion or impulsive decisions and ensure informed consent is given.
Source: TH
Read this in Hindi: यूके असिस्टेड डाइंग बिल
Previous article
Nuclear Non-Proliferation Treaty (NPT)
Next article
Understanding Pakistan’s Balancing Act on Iran