
In News
According to the World Health Organization (WHO), Antimicrobial resistance (AMR) is one of the greatest challenges of the 21st century.
About
- Since January 2020, there have been over three million deaths globally on account of COVID-19, starkly exposing the vulnerabilities of health systems to infectious disease.
- As serious as the current health and economic crisis is, COVID-19 can be the harbinger of future crises. And, one such major crisis is Antimicrobial Resistance (AMR).
- This could be the greatest challenge of the 21st century as amidst the pandemic there are rampant use of antibiotics (For example: Azithromycin & other antibiotics used by most of the people.)
What is Antimicrobial Resistance (AMR)?
- Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
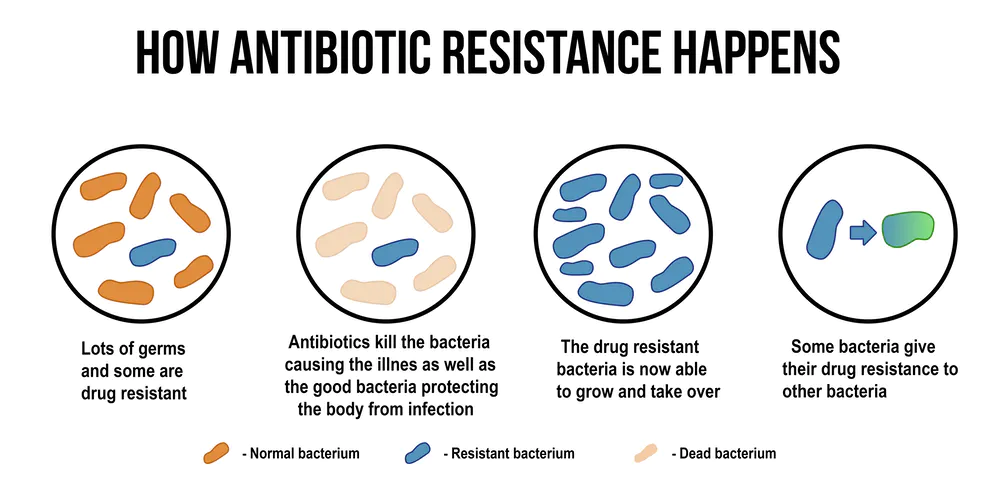
Image Courtesy: Conservation
- Emergence and spread of AMR
- AMR occurs naturally over time, usually through genetic changes.
- Antimicrobial-resistant organisms are found in people, animals, food, plants and the environment (in water, soil and air).
- They can spread from person to person or between people and animals, including from food of animal origin.
- The main drivers of antimicrobial resistance include the misuse and overuse of antimicrobials, lack of access to clean water, sanitation and hygiene (WASH) for both humans and animals, poor infection and disease prevention and control in healthcare facilities and farms, poor access to quality, affordable medicines, vaccines and diagnostics, lack of awareness and knowledge, and lack of enforcement of legislation.
Factors Causing AMR in India
- Inappropriate consumption of broad-spectrum (last resort) antibiotics is high because of changing prescription practice in the healthcare system due to the non-availability of a narrow spectrum of antibiotics.
- Inappropriate antibiotic use among the general public like Self-medication to avoid the financial burden.
- The large proportion of sewage is disposed of untreated into receiving water bodies, leading to gross contamination of rivers with antibiotic residues, antibiotic-resistant organisms.
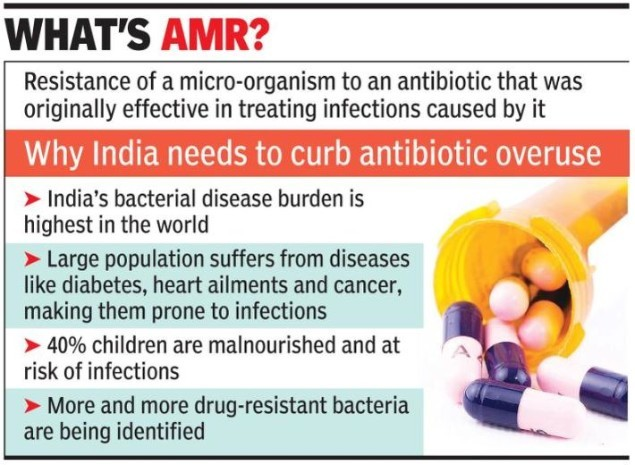
Image Courtesy: TOI
|
What are Antimicrobials?
|
Challenges Posed by AMR
- Antibiotic resistance is emerging as the threat to successful treatment of infectious diseases, organ transplantation, cancer chemotherapy and major surgeries.
- The issue of AMR causes out of pocket expenditure on health care, especially on medicines. The use of high order drugs or second-line expensive antibiotics pushing treatment cost high.
- Neonates and elderly both are prone to infections and are vulnerable.
Global Concerns
- It is a global health and development threat.
- WHO has declared that AMR is one of the top 10 global public health threats facing humanity. AMR is already responsible for up to 7,00,000 deaths a year.
- Unless urgent measures are taken to address this threat, we could soon face an unprecedented health and economic crisis of 10 million annual deaths and costs of up to $100 trillion by 2050.
- Antibiotics are becoming increasingly ineffective as drug resistance spreads globally leading to more difficult to treat infections and death.
- All these effects will be felt globally, but the scenario in the low- and middle-income countries (LMICs) of Asia and Africa is even more serious.
- LMICs have significantly driven down mortality using cheap and easily available antimicrobials. In the absence of new therapies, health systems in these countries are at severe risk of being overrun by untreatable infectious diseases.
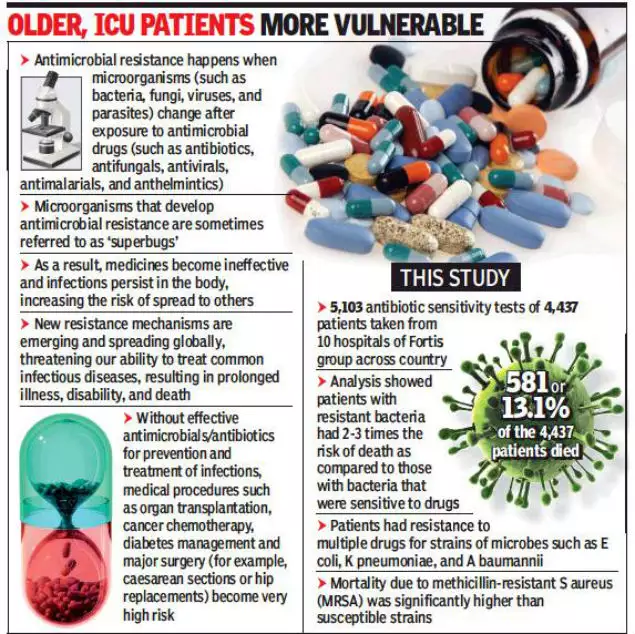
Image Courtesy: TOI
Various Initiatives Adopted In This Aspect
Global Efforts
- Global Action Plan on Antimicrobial Resistance (GAP): Globally, countries committed to the framework set out in the Global Action Plan1 (GAP) 2015 on AMR during the 2015 World Health Assembly and committed to the development and implementation of multisectoral national action plans.
- Tripartite Joint Secretariat on Antimicrobial Resistance: Tripartite joint secretariat (FAO, OIE and WHO) has been established and is hosted by WHO to drive multi-stakeholder engagement in AMR.
- Interagency Coordination Group (IACG) on AMR: It was convened by the Secretary-General of the United Nations after the UN High-Level Meeting on Antimicrobial Resistance in 2016.
- The IACG brought together partners across the UN, international organizations and individuals with expertise across human, animal and plant health, as well as the food, animal feed, trade to formulate a plan for the fight against antimicrobial resistance.
- World Antimicrobial Awareness Week (WAAW): WAAW was previously called the World Antibiotic Awareness Week. From 2020, it will be called the World Antimicrobial Awareness Week.
- It is a global campaign that aims to raise awareness of antimicrobial resistance worldwide.
- Global Antimicrobial Resistance and Use Surveillance System (GLASS): WHO launched it in 2015 to continue filling knowledge gaps and to inform strategies at all levels.
- GLASS has been conceived to progressively incorporate data from surveillance of AMR in humans, surveillance of the use of antimicrobial medicines, AMR in the food chain and the environment.
- Global Antibiotic Research and Development Partnership (GARDP): A joint initiative of WHO and the Drugs for Neglected Diseases Initiative (DNDi), GARDP encourages research and development through public-private partnerships.
- By 2025, the partnership aims to develop and deliver five new treatments that target drug-resistant bacteria identified by WHO as posing the greatest threat.
- Country wise initiatives:A multi-sectoral $1 billion AMR Action Fund was launched in 2020 to support the development of new antibiotics, and the U.K. is trialling a subscription-based model for paying for new antimicrobials towards ensuring their commercial viability.
- Peru’s efforts on patient education to reduce unnecessary antibiotic prescriptions.
- Australian regulatory reforms to influence prescriber behaviour, and initiatives to increase the use of point-of-care diagnostics, such as the EU-supported VALUE-Dx programme.
- Denmark’s reforms to prevent the use of antibiotics in livestock have not only led to a significant reduction in the prevalence of resistant microbes in animals, but also improved the efficiency of farming.
- India’s initiative
- To prevent the Over the counter sales of antibiotics, the central drug standard control organization(CDSO) prohibits medical stores from selling 24 key antibiotics without a doctor’s prescription.
- India’s Red Line campaign: Which demands that prescription-only antibiotics be marked with a red line, to discourage the over-the-counter sale of antibiotics– is a step forward.
- National Health Policy, 2017, terms antimicrobial resistance as one of the key healthcare issues and prioritizes the development of guidelines regarding antibiotic use and check on restricting the growth of antibiotics.
- The National Action Plan on Antimicrobial Resistance (NAP-AMR) 2017 has assigned coordinated tasks to multiple government agencies involving health, education, environment, and livestock to change prescription practices and consumer behaviour and to scale up infection control and antimicrobial surveillance.
- FSSAI has set certain guidelines limiting the antibiotics in food products such as fish and honey.
Conclusion & Way Forward
- Till now, there are two major possible solutions to combat the AMR menace:
- Discovery of new drugs, before the emergence of resistance in germs; and prudent use of available antibiotics.
- The discovery of a new drug is an expensive and unpredictable process, the estimated cost for developing a new antibiotic exceeds $1 billion.
- The second solution is the best possible solution i.e. to use the available antibiotics carefully to ensure their efficacy for as long as possible.
- Other steps: AMR requires a united multisectoral approach.
- Efforts to control prescription through provider incentives should be accompanied by efforts to educate consumers to reduce inappropriate demand, issue standard treatment guidelines.
- Policy alignment is also needed much beyond the health system. Solutions in clinical medicine must be integrated with improved surveillance of AMR in agriculture, animal health and the environment.
Previous article
New Fly Ash Utilisation Rule