Syllabus: GS2/Health
Context
- The World Health Organisation has published two new reports – ‘World Mental Health Today’ and ‘Mental Health Atlas 2024.’
- The reports serve as critical tools to shape global dialogue ahead of the 2025 United Nations High-Level Meeting on noncommunicable diseases and promotion of mental health and well-being, taking place in September 2025.
Major Highlights
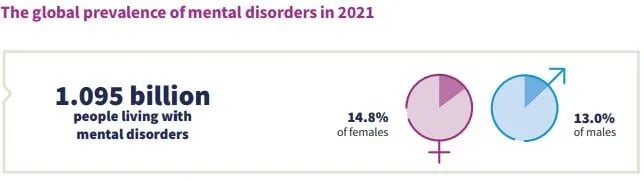
- Global Mental Health Issue: More than a billion people are living with mental health disorders.
- An estimated 727,000 people across all ages lost their lives to suicide in 2021, with one suicide death happening in over 20 suicide attempts.
- Suicide accounts for one in every 100 deaths globally.
- Most Common Mental Health Disorders: Anxiety and depressive disorders together accounted for more than two-thirds of all mental health conditions in 2021.
- Between 2011 and 2021, the number of people living with mental disorders increased faster than the global population.
- Vulnerable Age Groups: Younger adults aged 20–29 years are estimated to have the largest increases (1.8 percent) in prevalence since 2011.
- Males are estimated to have attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorders, and an idiopathic disorder of intellectual development more commonly.
- Females are estimated to experience anxiety, depressive, and eating disorders more often.
- Progress under SDG: Suicide is the leading cause of death among young people across all countries and socio-economic contexts.
- Yet, progress in reducing suicide mortality is too low to meet the United Nations Sustainable Development Goal (SDG) of a one-third reduction in suicide rates by 2030.
- Currently, only a 12% reduction will be achieved by that deadline.
- Economic and Policy Implications: While health-care costs are substantial, the indirect costs – particularly in lost productivity – are far greater.
- Depression and anxiety alone cost the global economy an estimated US$1 trillion each year.
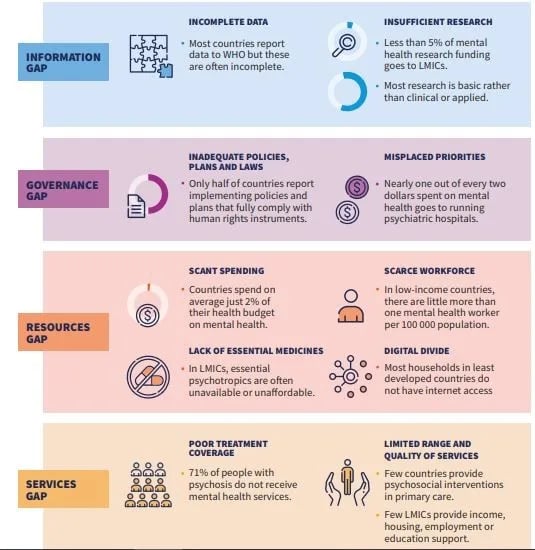
- Lack of Quality Care: Reaffirms continuing shortfalls in resources, workforce availability, and the quality of care, especially in low- and middle-income countries.
- Fewer than one in ten (9%) people with major depressive disorder have been estimated to receive minimally adequate treatment globally.
Key Gaps in Mental Health Transformation
Mental Health Concerns in India
- As per the National Mental Health Survey (NMHS) 2015-16,10.6% adults in India suffered from mental disorders, while the treatment gap for mental disorders ranged between 70% and 92%.
- The prevalence of mental morbidity was higher in urban metro regions (13.5%) as compared to rural areas (6.9%).
- The Economic Survey 2024-25 highlights the connection between mental health and the country’s economic future. The survey highlights the rising mental health concerns among India’s youth due to:
- Excessive internet & social media use: Leads to anxiety, sleep disorders, and attention issues.
- Lack of family engagement: Weak social support systems negatively impact emotional well-being.
- Hostile workplaces & long working hours: Cause burnout, stress, and reduced productivity.
- Unhealthy lifestyle choices: Ultra-processed foods and lack of physical activity worsen mental and physical health.
Challenges in Psychiatric Healthcare in India
- Poor Conditions in Psychiatric Hospitals: Often associated with cruelty, neglect, abuse, and substandard living conditions.
- Reflects systemic neglect and inadequate accountability mechanisms.
- Scant Funding: Mental health receives extremely low budget allocation, about 1% of the total health budget, with most going to institutions rather than community-based care.
- Shortage of Trained Personnel: Severe scarcity of psychiatrists, psychologists, counsellors, nurses, and social workers.
- Disproportionate distribution: Few psychiatrists at district HQs, almost none in towns/villages.
- This leads to an urban-rural mental healthcare divide.
- Accessibility & Economic Barriers: Medicines are unavailable in rural/interior areas.
- Travel to seek care leads to loss of wages, unaffordable for poor families.
- Patients with severe mental illness are usually non-earning members, worsening their financial strain.
Key Initiatives by the Government of India
- Mental Healthcare Act, 2017: The act decriminalised suicide attempts in India and also included WHO guidelines in the categorisation of mental illnesses.
- The most significant provision in the act was “advance directives”, which allowed individuals with mental illnesses to decide the course of their treatment.
- It also restricted the use of electro-convulsive therapy (ECT) and banned its use on minors, finally introducing measures to tackle stigma in Indian society.
- Rights of Persons with Disabilities Act, 2017: The Act acknowledges mental illness as a disability and seeks to enhance the Rights and Entitlements of the Disabled.
- Kiran Helpline: The helpline is a step towards suicide prevention and can help with support and crisis management.
- District Mental Health Programme (DMHP): Delivered in 767 districts, offering services like suicide prevention, stress management, and counseling.
- National Tele Mental Health Programme (NTMHP): Launched in 2022 to provide access to mental health services through 53 Tele MANAS Cells across 36 states/UTs.
- Expansion of Mental Health Capacity: Strengthening mental health services and educational resources in medical colleges and hospitals.
Source: IE
Previous article
India Sets Eyes on $1-Trillion Semiconductor Market