Kurukshetra October, 2025
The following topics are covered in the Kurukshetra October 2025:
Chapter 1- Rashtriya Poshan Maah
Malnutrition in India remains a multidimensional challenge impacting health, productivity, and economic growth. Globally, it costs the economy US$3.5 trillion annually, or about US$500 per person, underscoring that nutrition is not just a health issue but an economic necessity.
- India’s fight against malnutrition has evolved over decades, beginning with the Integrated Child Development Services (ICDS) in 1975, one of the world’s largest community-based programmes delivering health, nutrition, and early childhood education services to children under six, pregnant women, and lactating mothers.
Evolution of India’s Nutrition Policy
POSHAN Abhiyaan (2018)
Launched in 2018, the POSHAN Abhiyaan (National Nutrition Mission) marked a paradigm shift in India’s nutrition strategy, focusing on the first 1,000 days of life — from conception to a child’s second birthday.
It rests on a three-pronged approach:
- Jan Andolan: Community-led behaviour change campaigns.
- Digital Monitoring: Real-time service tracking via the POSHAN Tracker.
- Capacity Building: Training 1.4 million Anganwadi Workers through the Incremental Learning Approach (ILA).
To strengthen convergence, the Government launched Saksham Anganwadi and Mission Poshan 2.0 in 2021, integrating POSHAN Abhiyaan, Anganwadi Services, and the Scheme for Adolescent Girls. Functional across 28 States and 8 UTs, it now serves nearly 10 crore beneficiaries, delivering Supplementary Nutrition, Growth Monitoring, and Behaviour Change Communication (BCC).
Rashtriya Poshan Maah: The SBCC Engine
Introduced in September 2018 as part of the Jan Andolan, Rashtriya Poshan Maah serves as the annual focal point of a year-round Social Behaviour Change Communication (SBCC) and service delivery framework.
It translates policy ambition into household practice through coordinated action among communities, local governance institutions, and frontline systems.
SBCC Strategy
Poshan Maah uses a three-tier communication approach:
- Mass Media: TV, radio, and digital platforms for large-scale outreach.
- Mid-Media: Local radio, wall paintings, folk performances, and school activities for community engagement.
- Interpersonal Counselling: Home visits and awareness drives by Anganwadi Workers using digital tools.
This ensures participation from mothers, fathers, adolescents, teachers, Panchayat leaders, and community influencers.
Journey of Poshan Maah: 2018–2025
| Year | Theme / Focus | Theme / Focus |
|---|---|---|
| 2018 | Launch Year | Awareness drives in schools, communities, Anganwadis – foundation for Jan Andolan. |
| 2019 | Poshan Tyohar Se Vyavahar | Emphasised translating celebration into healthy behaviour; focus on first 1,000 days, anaemia, diarrhoea, sanitation, and dietary diversity. |
| 2020 | Digital Outreach during COVID-19 | Use of e-Samvads, webinars, social media campaigns, and promotion of Poshan Vatikas (nutri-gardens). |
| 2021 | Thematic Weekly Activities (Azadi Ka Amrit Mahotsav) | Plantation drives, yoga-based awareness, nutrition kit distribution. |
| 2022 | Panchayat-led Poshan Maah | Focus on Mahila aur Swasthya and Bacha aur Shiksha; organisation of Poshan Panchayats, tribal food promotion, recipe exhibitions. |
| 2023 | Life-cycle Approach | Integration of health, education, and nutrition; focus on diet diversity, anaemia prevention, and technology-enabled governance. |
| 2024 | Consolidation Phase | Focus on anaemia prevention, growth monitoring, complementary feeding, Poshan Bhi Padhai Bhi, and digital service delivery. |
| 2025 | Swasth Naari, Shashakt Parivar | Focus on obesity prevention, reduced sugar-salt-oil intake, ECCE, IYCF, men’s participation, and convergence across sectors. |
Over time, Poshan Maah has transformed from a limited awareness drive into one of India’s largest peopleled movements, engaging crores of citizens annually and creating a culture of nutrition awareness and local accountability.
Significance of Rashtriya Poshan Maah
- Behavioural Transformation: Moves beyond information dissemination to foster sustained social behaviour change through community engagement.
- Convergence Platform: Aligns multiple ministries and programmes — Health, Education, Jal Shakti, Rural Development, and Panchayati Raj — ensuring holistic service delivery.
- Community Ownership: Empowers local governance institutions, especially Gram Panchayats, to lead nutrition campaigns.
- Technology-Enabled Governance: Use of digital dashboards, mobile-based monitoring, and the POSHAN Tracker ensures transparency and accountability.
- Economic and Human Development Impact: Improved nutrition enhances productivity, reduces healthcare costs, and contributes to human capital formation.
Challenges Ahead
- Regional Disparities: Malnutrition indicators vary widely across states, with higher prevalence in tribal and rural areas.
- Behavioural Inertia: Deep-rooted cultural food practices and gender biases limit adoption of improved nutrition habits.
- Supply Chain Gaps: Irregular supply of supplementary nutrition and weak last-mile monitoring affect outcomes.
- Convergence Deficit: Coordination among departments remains uneven across states.
Way Forward
- Strengthen Last-Mile Delivery: Ensure seamless supply of supplementary nutrition through technologybased tracking.
- Men-streaming Nutrition Awareness: Engage men as active participants in family nutrition and child health.
- Promote Local Food Systems: Encourage dietary diversity through local, seasonal, and traditional food practices.
- Institutionalise SBCC: Integrate nutrition and health communication modules in school and Panchayatlevel training.
- Measure and Review: Use Poshan Maah as an annual evaluation point for progress, innovation, and course correction.
Chapter 2- Nourishing India’s Future
Nutrition and early childhood care form the foundation of a nation’s human capital. India’s flagship POSHAN Abhiyaan (2018) reflects this vision, aiming to reduce malnutrition through convergence, technology, and behaviour change communication.
- The 8th Rashtriya Poshan Maah (September 2025) highlights themes such as Infant and Young Child Feeding (IYCF), Early Childhood Care and Education (ECCE), and Nutrition Literacy to Tackle Obesity, aligning with the goal of a Suposhit and Viksit Bharat by 2047.
1. Infant and Young Child Feeding (IYCF)
Why Early Nutrition Matters
The first 1,000 days — from conception to age two — determine lifelong health, cognitive ability, and productivity. According to WHO, indicators like stunting and wasting often emerge in the first six months, underscoring the importance of timely feeding practices.
Exclusive Breastfeeding: The Superfood Advantage
- Exclusive breastfeeding for the first 6 months is both traditional wisdom and a scientifically proven intervention against infections, malnutrition, and infant mortality.
- Breast milk provides antibodies, nutrients, and growth factors, reducing risks of asthma, obesity, and diabetes.
- For mothers, it lowers risks of breast and ovarian cancers and type-2 diabetes.
- WHO advises initiating breastfeeding immediately after birth to ensure immunity and survival.
The Ministry of Women and Child Development (MoWCD) promotes IYCF through Anganwadi home visits and Social and Behaviour Change Communication (SBCC) under Mission Saksham Anganwadi and Poshan 2.0, counselling families on optimal feeding.
Complementary Feeding (6–24 months)
Beyond six months, a child’s nutritional needs surpass what breast milk provides. The WHO recommends:
- 6–8 months: 2–3 small meals plus breastfeeding
- 9–24 months: 3–4 meals + 1–2 nutritious snacks daily
Dietary diversity is crucial — meals should include cereals, pulses, milk, eggs, meat/fish, fruits, and vegetables while limiting sugar, salt, and oils.
The Annaprashan Diwas initiative celebrates the introduction of complementary foods, promoting local, low-cost recipes rooted in tradition and science.
Responsive Feeding and Shared Responsibility
Nutrition is more than food — it is responsive caregiving, involving emotional bonding and interactive feeding. Studies show this practice:
- Builds healthy food preferences,
- Reduces undernutrition and obesity risks, and
- Fosters emotional and cognitive growth.
Through Jan Andolan-style campaigns, the government ensures families adopt IYCF practices — exclusive breastfeeding for 6 months, timely complementary feeding, and responsive caregiving — to break the intergenerational cycle of malnutrition.
2. Early Childhood Care and Education (ECCE)
Constitutional and Policy Framework
- The 86th Constitutional Amendment (2002) inserted Article 45, directing the State to provide ECCE for all children up to six years.
- The RTE Act (2009) extended this through Section 11, mandating free pre-school education for children above three years.
- ECCE ensures holistic development — physical, cognitive, emotional, and social — making children school-ready, resilient, and developmentally on track.
ECCE within Mission Saksham Anganwadi and Poshan 2.0
The Anganwadi network (over 14 lakh centres, reaching 46% of India’s under-six population) remains the world’s largest early childhood development programme.
Originally for Below Poverty Line families, it was universalised in 2009 to ensure free access to nutrition, health services, and preschool education for all.
The Saksham Anganwadi and Poshan 2.0 scheme aims to transform Anganwadis into vibrant early learning hubs with improved infrastructure and training.
Poshan Bhi Padhai Bhi (PBPB) Initiative
Launched on 10 May 2023, PBPB integrates play-based, inclusive ECCE at Anganwadi Centres.
- Training: 14 lakh Anganwadi Workers are being trained (5 days each) through a two-tier model by SPNIWCD (formerly NIPCCD); over 7 lakh workers are already trained.
- Curricula:
- Navchetana – National Framework for Early Childhood Stimulation (birth–3 years).
- Aadharshila – National Curriculum for ECCE (3–6 years).
- Digital Support: Daily ECCE activity videos and voice notes via the Poshan Tracker app guide Anganwadi workers with low-cost, play-based learning materials.
- Recognition: Children completing ECCE receive an ECCE Certificate, linked to APAAR ID and UDISE databases for continuity into formal schooling.
- Co-location guidelines ensure Anganwadi Centres function alongside government primary schools.
Community and Behavioural Outreach
Monthly events like Sports Day, Creativity Day (Nanhe Kalakaar), and Annual Day engage parents and local communities.
Campaigns during Poshan Maah (September) and Poshan Pakhwada (March) promote awareness through Shiksha Chaupal, DIY toy fairs, and play-based demonstrations.
This community-based model underscores that “play is learning”, shaping empathy, curiosity, and lifelong learning.
3. Advancing Nutrition Literacy to Tackle Obesity
The Emerging Challenge
As India reduces undernutrition, overnutrition and obesity are emerging as twin threats. The Household Consumption Expenditure Survey (HCES) shows processed foods and beverages now dominate food spending across rural and urban India.
Unhealthy dietary shifts, sedentary lifestyles, and digital habits are fuelling a public health crisis involving obesity, diabetes, and cardiovascular diseases.
Health and Socioeconomic Impacts
- Among children: low self-esteem, teasing, early-onset diabetes, and cardiac risks.
- Among adults: higher incidence of PCOS, infertility, cancers (colon, breast, liver), and cognitive decline.
- Economic effects include reduced productivity and higher healthcare costs, perpetuating intergenerational obesity
Policy and Behavioural Response
The 8th Poshan Maah (2025) emphasizes nutrition literacy — empowering citizens to make informed food choices through SBCC and community engagement.
Key public messages include:
- Regular weight monitoring to track nutrition status.
- Limit salt, sugar, and oils; prefer local, balanced meals.
- Read food labels, practice mindful eating, and ensure adequate sleep.
- 60 minutes of daily physical activity or yoga and reduced screen time.

To drive awareness, the MoWCD has introduced “Oil and Sugar Boards” at Anganwadi Centres — visual tools prompting families to reflect on daily consumption patterns and adopt moderation.
Chapter 3- Nutrition Sensitive Agriculture in Rural India
In rural India—home to nearly 900 million people, where agriculture employs 44% of the workforce— Nutrition Sensitive Agriculture (NSA) integrates farming and nutrition to address undernutrition, micronutrient deficiencies, and obesity. By promoting biofortified crops, dietary diversity, women’s empowerment, and climate-resilient farming, NSA directly contributes to SDG 2 (Zero Hunger) and SDG 3 (Good Health and Well-being).
India’s Nutrition Paradox
Despite being the world’s largest milk producer (220 million tonnes) and a major exporter of pulses and spices, India faces severe malnutrition.
- Global Hunger Index 2024: Rank 105/127, score 27.3 (“serious”).
- NFHS-5 (2019–21): 35.5% of children under 5 are stunted, 19.3% wasted, and 67.1% anaemic. Monotonous cereal-based diets dominate rural areas, eroding nutritional outcomes.
Concept and Core Elements
According to FAO, NSA strengthens agricultural systems to improve nutrition outcomes through diversification, equity, and health linkages.
Key Components:
- Crop diversification: Millets, pulses, fruits, and vegetables.
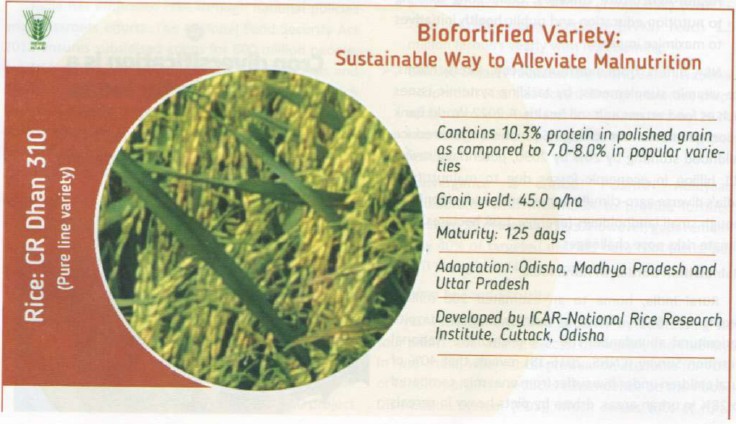
- Biofortification: Zinc-rich wheat, iron-fortified millets, vitamin A sweet potatoes.
- Women’s empowerment: Women form 70–80% of the agricultural workforce but own <13% of land (World Bank, 2020).
- Health linkages: Nutrition education and convergence with public health schemes.
World Bank (2022) estimates NSA could reduce child stunting by 20% by 2030, saving $11 billion in malnutrition-related losses.
Rural Nutrition Burden
- CNNS (2016–18): 40% of rural children under five are anaemic (vs 28% urban).
- SOFI 2023: 224 million Indians (16.6%) undernourished.
- Rural poverty: 19.28% (NITI Aayog MPI, 2023).
- Micronutrient deficiencies:
- Zinc deficiency in 30% of preschoolers.
- Vitamin A deficiency causes blindness in 6.1 million children annually (WHO 2023).
- 54.3% of pregnant women anaemic, leading to 18.2% low birth weight infants.
Climate stress: Erratic rainfall reduced pulse output by 15% in rainfed areas (ICAR 2024). Post-harvest losses reach 40% for perishables (FAO 2023).
Economic loss: 4% of GDP annually (~$1.4 trillion, World Bank 2019).
Implementation in India
NSA has been integrated into several national policies and missions:
- POSHAN Abhiyaan (2018): Targets 2% annual reduction in stunting.
- Biofortification Mission (2022–25): ₹10,000 crore to promote nutrient-rich crops for 10 million farmers.
- ICAR “Seeds for Nutrition” (2020): Distributed 50 million seed packets; 30% rise in iron-fortified millet cultivation in Rajasthan.
- FAO Project (Madhya Pradesh): Dairy intake up 25%, child anaemia down 15% (2023).
- UNICEF “Nutrition-Smart Villages” (Bihar): 15,000 women trained; dietary diversity up from 3.5 to 4.7 food groups (2023).
- World Bank Climate Plan (Maharashtra): Drought-tolerant crops across 2 million ha raised yields by 20%. Yet, only 40% of targeted districts have operational NSA plans (NITI Aayog 2024).
Food Security Dimensions
1. Availability:
- HarvestPlus (2017–23): 15 million farmers adopted vitamin A-enriched maize/potatoes, increasing nutrient availability by 10–15% (IFPRI 2023).
- Tamil Nadu’s millet mission raised production to 1.5 million tonnes.
2. Access:
- Women’s SHGs under NRLM saw income rise 20–30%.
- World Bank (2022): 18% higher spending on diverse foods among SHG households in UP.
3. Utilisation:
- USAID (2023): Jharkhand households’ child nutrient intake rose 22% through local superfood recipes.
4. Stability:
- CGIAR (2024): Stabilised yields in 10 states; seasonal hunger down 12%.
- Hunger Watch (2023): NSA households 25% less likely to face food shortages.
Health and Economic Impact
- Kerala: NSA districts show 15% lower stunting than Bihar (NFHS-5).
- Odisha (IFPRI 2022): Iron-fortified crops reduced anaemia by 16%, improved cognition by 8%.
- Punjab (WHO 2023): Livestock-based NSA cut vitamin D deficiency by 20%.
- UNICEF 2024: 10% fewer preterm births with improved folate intake.
- Lancet 2023: NSA scaling could prevent 1 million child deaths by 2030, boost rural GDP by 2–3%.
- NIMHANS 2024: 15% decline in women’s depression rates in NSA communities.
Case Studies
- Rajasthan (Bundi): BAIF–FAO’s “Nourish the Future” (2019–24) — dietary diversity up from 2.8→5.2 food groups, stunting down 12%, incomes up 28%.
- Andhra Pradesh (RySS): Watershed-linked NSA boosted vegetable yield by 35%, anaemia fell 22% (World Bank 2023).
- Kerala: NSA in 80% panchayats reduced underweight children by 18% (2024). Digital innovations like the POSHAN Tracker now monitor 100 million nutrition records monthly.
Challenges and Future Pathways
- NSA receives only 5% of agriculture budgets; outreach covers 30% of smallholders (ICRIER 2024).
- Persistent gender inequities and weak inter-ministerial convergence.
Way Forward:
- Expand digital and AI-based crop-nutrition advisories.
- Strengthen public–private partnerships.
- National Agriculture Policy 2025 (draft): ₹2.5 lakh crore to scale NSA, targeting 50% dietary diversity coverage by 2030.
- Collaboration with CGIAR India Hub (2024) for innovation and capacity building
Chapter 4- Digital Transformation in Healthcare
India’s healthcare sector stands at a critical juncture. Over the past decade, there has been a surge in digital health innovations — telemedicine, electronic health records (EHRs), wearable technologies, and health-tech startups — along with government reforms like the Ayushman Bharat Digital Mission (ABDM).
- These aim to make healthcare accessible, efficient, and equitable, particularly for rural India, where malnutrition and disease remain deeply interconnected.
- Globally, the COVID-19 pandemic accelerated digital health adoption. The WHO noted how nations like Singapore and South Africa relied on telemedicine during lockdowns.
- India’s CoWIN platform became a model of digital deployment for a billion-plus population, proving digital health is both feasible and necessary.
National Digital Initiatives
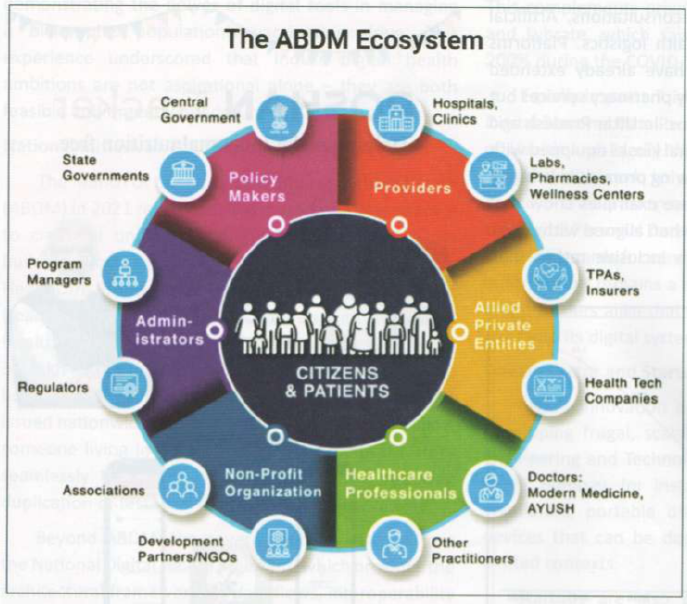
The Ayushman Bharat Digital Mission (ABDM), launched in 2021, seeks to create a unified digital health infrastructure. Its pillars include:
- Health Facility Registry,
- Healthcare Professionals Registry,
- Ayushman Bharat Health Account (ABHA), and
- Unified Health Interface (UHI).
As of August 2025, over 3.3 lakh facilities and 4.7 lakh professionals are registered, with millions of ABHA IDs issued, enabling seamless transfer of medical records nationwide.
The National Digital Health Blueprint (NDHB) provides the framework for interoperability and secure data exchange, envisioning a “digital health highway” for citizens.
The eSanjeevani telemedicine platform has delivered over 150 million consultations, making it the world’s largest telemedicine initiative. Private platforms like Practo and Lybrate saw consultations rise by 200% during COVID-19.
The Digital Personal Data Protection Act (2023) and Health Ministry guidelines now safeguard patient data and consent — crucial for building trust in digital health systems.
Private Sector and Innovation
The Biomedical Engineering and Technology Innovation Centre (BETIC) at IIT Bombay has developed low-cost ventilators, portable dialysis units, and point-of-care devices suited for rural India.
Indian health-tech startups attracted nearly USD 1.2 billion (2021–23) in funding across teleconsultation, AI diagnostics, and logistics. Firms like 1mg and PharmEasy expanded to tier-II and rural regions, offering e-consultations and diagnostics.
Pilot “Health ATMs” in Uttar Pradesh and Bihar — digital kiosks with diagnostic tools — are bridging rural health gaps, proving the impact of public–private synergy.
Digital Health and Rural India
According to NFHS-5, 35.5% of children under five are stunted, and 57% of women (15–49) are anaemic. Digital tools can help address these issues:
- Frontline empowerment: Apps for ASHA and Anganwadi workers track anaemia and immunisation in real time.
- POSHAN Tracker: Integrates nutrition data for targeted interventions.
- Example: An Anganwadi worker in Madhya Pradesh used it to identify a severely anaemic girl, ensuring timely care.
- Tele-nutrition counselling: Connects mothers in rural areas to nutritionists.
State-wise contrasts — 42% stunting in Bihar vs 23% in Kerala — show the need to integrate nutrition data into ABDM for focused resource allocation.
Challenges
- Provider adaptation: Many doctors and nurses lack digital training.
- Connectivity gaps: Rural internet penetration (TRAI, 2023) is 38%, compared to 70% in urban India.
- Privacy risks: Data misuse can erode trust, as seen in the UK’s Care.data failure (2016).
- Fragmentation: Multiple non-interoperable platforms hinder efficiency.
- AI caution: Biased algorithms may compromise diagnostics.
Global experiences — Singapore’s HealthHub and New Zealand’s digital insurance model — show that technology must be paired with governance, data standards, and trust.
Way Forward
- Build interoperable EMRs with open APIs and consent-driven access.
- Strengthen capacity building for ASHAs, ANMs, and clinicians.
- Expand public–private partnerships for telemedicine kiosks and IoT-based health ATMs.
- Integrate nutrition and health data into national dashboards.
- Use digital surveillance to predict disease outbreaks linked to climate change.
Case Studies
- eSanjeevani: 150+ million consultations.
- Delhi’s Health Information Management System: Reduced OPD waiting times.
- KLES Hospital, Belagavi: Fully paperless system reduced errors.
- Andhra Pradesh Real-Time Monitoring System: Tracks maternal health, reducing referral delays.
- POSHAN Tracker: Nationwide tool for monitoring nutrition outcomes.
UPSC Mains Practice Questions-(Around 250 words)
Q1. Discuss the causes of India’s growing water crisis and critically evaluate the effectiveness of policy interventions such as the Jal Jeevan Mission and Atal Bhujal Yojana
Q2. Artificial Intelligence and automation are reshaping the employment structure in India. Examine their implications for inclusive growth and policy responses required.
QUICK LINKS